Benign prostatic hyperplasia is a common health condition when men get older. The enlarged prostate gland causes a number of unpleasant urinary symptoms, including blocking the urine flow. The good news is that there are some effective treatments, such as special meds, surgeries, and minimally invasive therapies. To make the best choice, consider symptoms, prostate size, and other conditions.
Benign Prostatic Hyperplasia Symptoms
Their severity varies, but signs tend to worsen over time. The most common ones include: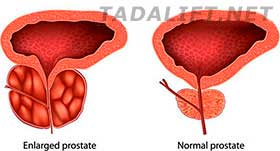
- Urgent or frequent needs to urinate;
- Inability to empty the bladder completely;
- Difficulty starting urination;
- Dribbling at the end of this process;
- Weak urine stream;
- Increased frequency of night urination;
- Stream that starts and stops.
There are other less common symptoms of benign prostatic hyperplasia, such as:
- Blood in the urine;
- Inability to urinate;
- Urinary tract infections.
Effective Treatment Options
 If you experience any urinary issues, you need to see your doctor because it’s necessary to identify underlying causes and treat this health condition. There are many treatment options available to men with benign prostatic hyperplasia, but the right choice depends on your age, prostate size, overall health, etc.
If you experience any urinary issues, you need to see your doctor because it’s necessary to identify underlying causes and treat this health condition. There are many treatment options available to men with benign prostatic hyperplasia, but the right choice depends on your age, prostate size, overall health, etc.
The intake of specific medications is the most common treatment for moderate and mild symptoms. Available options include alpha blockers, tadalafil, 5-alpha reductase inhibitors, and combined drug therapy. That’s because these drugs relax prostate and bladder muscles and shrink the prostate by preventing hormonal changes, thus, making urination easier.
Surgical or minimally invasive therapies are recommended if men have severe or moderate symptoms, medications don’t help, they prefer a definitive treatment, and have bladder stones, kidney issues or urinary tract obstruction. However, it’s not the best option for men with urethral stricture disease, untreated urinary tract infections, neurological disorders, and prostate radiation therapy history. Only doctors can determine the most suitable and effective BPH treatment.

