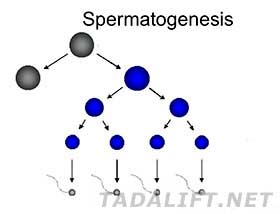
Spermatogenesis is the process in the male organism, which can be defined as the transformation of germ cells to spermatozoa. It develops in the testes seminiferous tubules and is usually divided into several stages, related to various germ cell types:
 Proliferation stage, which is characterized by the transformation of spermatogonia into spermatocytes. The stem, which is located within the basal area of the tubular epithelium, undergoes mitosis. Following the progeny of such divisions, they keep their numbers and advance to numerous interconnected B spermatogonia. They, in turn, divide and enhance to primary spermatocytes. All of the B spermatogonium descendants are related by cytoplasmic bridges that form a syncytium-like cells that undergo synchronous development;
Proliferation stage, which is characterized by the transformation of spermatogonia into spermatocytes. The stem, which is located within the basal area of the tubular epithelium, undergoes mitosis. Following the progeny of such divisions, they keep their numbers and advance to numerous interconnected B spermatogonia. They, in turn, divide and enhance to primary spermatocytes. All of the B spermatogonium descendants are related by cytoplasmic bridges that form a syncytium-like cells that undergo synchronous development;- Meiotic stage that is associated with spermatocytes transition to spermatids. Every spermatocyte is divided in order to advance to two secondary spermatocytes that give the rise to two other spermatids. Each spermatid contains a haploid quantity of chromosomes.
 The meiosis develops over a considerable period of time, with its first phase taking around three weeks;
The meiosis develops over a considerable period of time, with its first phase taking around three weeks;- Differentiation stage, when spermatids become spermatozoa. The phase is frequently called spermiogenesis. The three main changes that take place during this stage include acrosome formation, nuclear chromatin condensation and tail growth.
Contrary to female gametes production that appears fully before birth, males produce gametes right after puberty beginning onwards up to the end of their reproductive life. The main sites of spermatogenesis are seminiferous tubules, which are also divided into two types of cells involved in the process:
- Germ cells that develop into sperm;
- Somatic cells that nurture germ cells during the process of development.
Considering the hormonal control over spermatogenesis, it can be controlled by a range of mechanisms that usually involve testes, hypothalamus, and anterior pituitary. With the help of gonadotrophic releasing hormone, testosterone and oestrogen impact negatively on the hypothalamus and anterior pituitary, suppressing the secretion of the GnRH hormones.

