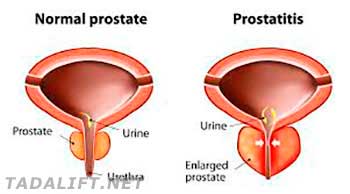
Prostatitis is a drastic condition, which triggers inflammation, excess tenderness and swelling of the prostate gland. The condition is frequently painful and ultimately felt during ejaculation and peeing. Unfortunately, there is no definite cause of the condition, specified by medical specialists, but urinary tract infection is often to blame. Besides, in a considerable part of times, a real cause of the disorder occurrence is not found. On the other hand, prostatitis has no definite cause but presupposes a challenging treatment, which can take months and years.
However, prevention is always a certain and dependable way to eliminate the condition development and warn its aggravations. Specific lifestyle changes, diversifications of the daily routine and diet plan can help you keep the prostate gland in a good condition and manage certain disorders. Additionally, such changes will help you decrease the risk of prostatitis development. Moreover, patients, who have already got prostatitis-related issues, can use life changes to ease the disorder and prevent more serious complications.
Top 5 Recommendations for Successful Prostatitis Prevention
While medications and treatments can help you eliminate the existing symptoms of the prostate gland abnormalities, preventative measures will help you eliminate the risk of the condition appearance. Follow simple tips to ensure good male health:
- Hygiene is a key to success. Prevent the infection by cleaning the penis and surrounding area;
- Prefer standing than sitting. Bike or bicycle rides, sedentary lifestyle and related issues can create abnormal pressure on your prostate gland, leading to inflammation;
- Consume more veggies and fruits, as they are ultimately high in nutrients that prevent inflammation and infection;
- Limit alcohol and caffeine consumption. Alcoholic beverages, coffee, soda, and tea can advance the risk of urinary tract inflammation;
- Obesity as prostate health enemy. Keep to a healthy diet, stay active and get enough sleep to prevent abnormalities.

