White spots on testicles are a common condition that many men notice at some point in their lives. Though finding unusual marks on such a sensitive area can cause concern, most cases are harmless and resolve without medical intervention. This article explains the different causes of white spots on the scrotum, when to seek medical attention, and effective treatment options.
Common Causes Of White Spots On Testicles
The male genital area, particularly the scrotum, has unique skin characteristics that make it prone to various skin conditions. Here are the most frequent causes of white spots that appear on the testicles:
Fordyce Spots
Fordyce spots are small, painless, white or yellowish bumps that appear on the scrotum. These spots are actually enlarged sebaceous glands and are completely normal variations of human anatomy.
Key characteristics:
- 1-3mm in size
- Painless and don’t itch
- May appear in clusters
- Natural occurrence, not an infection
- No treatment needed
Many men have Fordyce spots without realizing they’re a normal skin feature. These white dots on testicles affect around 80% of adults to some degree.

Ingrown Hair
When hair grows back into the skin instead of rising up from the follicle, it can cause white bumps on the scrotum. This is especially common in men who shave or trim their pubic hair.
Symptoms of ingrown hair:
- White or red bumps around hair follicles
- Mild pain or tenderness
- Possible itching
- Small amount of pus may be visible
Ingrown hairs typically resolve without treatment, though they can be uncomfortable. The white pimples on testicles caused by ingrown hairs should not be popped, as this can lead to infection and scarring.
Folliculitis
Folliculitis occurs when hair follicles become inflamed, often due to bacterial or fungal infection. The groin area is particularly susceptible because of warmth, moisture, and friction.
Signs of folliculitis:
- White or red bumps centered around hair follicles
- Itching and burning sensation
- Tenderness or pain
- Multiple bumps that may be filled with pus
Mild folliculitis often clears up with improved hygiene practices. More severe cases might require medical treatment with topical or oral antibiotics.
Pimples And Whiteheads
Just like elsewhere on the body, the skin on the scrotum can develop pimples when pores become clogged with oil and dead skin cells.
Characteristics of genital pimples:
- White or red bumps with a white center
- Slight pain when touched
- Isolated occurrences rather than clusters
- May come and go
These white bumps on balls are usually harmless and disappear on their own. As with facial acne, avoiding squeezing or popping these lesions is important to prevent infection.
Fungal Infections
The warm, moist environment of the groin makes it an ideal breeding ground for fungal infections, which can cause white patches in the groin area.
Common fungal infection symptoms:
- White or red rash with defined borders
- Intense itching, especially at night or after sweating
- Burning sensation
- Flaking or peeling skin
- May spread to nearby skin areas
Jock itch (tinea cruris) is a common fungal infection that can present with white spots or patches on the scrotum and surrounding areas. These infections typically respond well to over-the-counter antifungal treatments.
Molluscum Contagiosum
This viral infection causes small, flesh-colored or white bumps on the skin that have a characteristic dimple in the center.
Identifying features:
- Pearl-like appearance
- 2-5mm in size
- Painless with possible mild itching
- May appear in groups
- Can spread through direct contact
Molluscum contagiosum can affect any skin area, including the genitals. While harmless, the infection is contagious and may spread through sexual contact or shared towels and clothing.
Genital Warts
Caused by certain strains of human papillomavirus (HPV), genital warts can appear as white or flesh-colored bumps on the testicles and surrounding areas.
Characteristics of genital warts:
- Raised, cauliflower-like appearance
- May be white, pink, or flesh-colored
- Can appear individually or in clusters
- Usually painless but may itch
- Can spread through sexual contact
Unlike many other causes of white spots on testicles, genital warts represent a sexually transmitted infection that requires medical attention.
Less Common Causes Of White Spots On Scrotum
While most white spots on testicles are harmless, some less common conditions require medical evaluation:
Lichen Sclerosus
This chronic skin condition causes thin, white patches on the genitals that can become itchy, painful, and prone to tearing.
Signs of lichen sclerosus:
- White patches with wrinkled appearance
- Skin feels thin and papery
- May cause pain, especially during erection
- Can lead to scarring if untreated
Lichen sclerosus requires medical treatment, usually with topical corticosteroids, to manage symptoms and prevent complications.
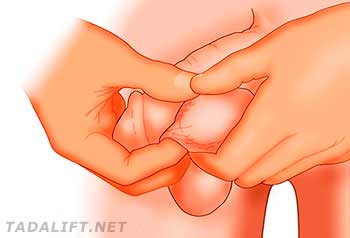
Sebaceous Cysts
These are small, slow-growing bumps under the skin that form when a sebaceous gland becomes blocked.
Key features:
- Firm, white lumps under the skin
- Range from pea-sized to larger
- Generally painless unless infected
- May have a central pore
- Contents may be cheese-like if squeezed
While usually harmless, infected sebaceous cysts may require medical treatment or drainage.
Herpes Simplex Virus
In some cases, herpes can cause white blisters on the scrotum that later rupture and form ulcers.
Herpes symptoms:
- Small groups of painful blisters
- Sores that rupture and weep
- Pain, itching, and burning
- Flu-like symptoms during first outbreak
- Recurrent episodes
Herpes is a sexually transmitted infection that requires medical diagnosis and treatment with antiviral medications.
Treatment Options For White Spots On Testicles
Treatment depends entirely on the underlying cause:
Home Remedies And Self-Care
For minor conditions like ingrown hairs, folliculitis, or mild fungal infections:
- Maintain good hygiene with daily washing using mild soap
- Wear clean, breathable cotton underwear
- Apply warm compresses to relieve discomfort
- Use over-the-counter antifungal creams for suspected fungal infections
- Avoid tight-fitting clothing that causes friction
- Don’t shave the area until the condition resolves
Medical Treatments
For more serious or persistent conditions:
- Antibiotics: Oral or topical for bacterial folliculitis or infected cysts
- Antifungal medications: For fungal infections like jock itch
- Antivirals: For viral infections like herpes or molluscum contagiosum
- Corticosteroids: For inflammatory conditions like lichen sclerosus
- Minor surgical procedures: For removal of cysts or warts
Prevention Of White Spots On Testicles
While not all causes can be prevented, these practices help reduce your risk:
- Maintain good genital hygiene
- Wear clean, breathable underwear
- Change out of wet or sweaty clothes promptly
- Use proper shaving techniques if you groom the area
- Practice safe sex to prevent STIs
- Avoid sharing personal items like towels
- Keep the area dry, especially in hot weather or after exercise
The Psychological Impact Of White Spots On Testicles
Finding unusual marks on the genitals can cause significant anxiety for many men. This anxiety is normal but often unnecessary, as most white spots on testicles are completely harmless.
If concerns about genital appearance or health are causing distress, speaking with a healthcare provider can provide reassurance and accurate information. Remember that variations in genital appearance are entirely normal.
FAQs About White Spots On Testicles
Are white spots on testicles common?
Yes, white spots on testicles are quite common. Many men have naturally occurring Fordyce spots, while temporary conditions like ingrown hairs or pimples affect most men at some point in their lives.
Can stress cause white spots on balls?
Stress itself doesn’t directly cause white spots, but it can weaken your immune system, potentially making you more susceptible to infections that might cause white spots. Stress can also worsen existing skin conditions.
Do white bumps on scrotum go away on their own?
Many causes of white bumps on the scrotum, such as pimples, ingrown hairs, and mild folliculitis, resolve on their own with proper hygiene. However, conditions like genital warts, herpes, or lichen sclerosus require medical treatment.
Is it normal to have white dots on testicles?
Yes, many men have small white dots called Fordyce spots on their testicles. These are enlarged sebaceous glands and represent a normal variation in anatomy rather than a medical condition.
Can poor hygiene cause white spots on testicles?
Yes, inadequate hygiene can contribute to several conditions that cause white spots, including fungal infections and folliculitis. Regular washing with mild soap can help prevent these issues.
Are white bumps on testicles contagious?
Most causes of white bumps on testicles are not contagious. However, certain conditions like molluscum contagiosum, genital warts, and herpes can spread through direct skin contact, including sexual activity.
How can I differentiate between normal white spots and an STI?
STIs often cause additional symptoms beyond just white spots, such as pain, unusual discharge, fever, or lymph node swelling. STI-related spots tend to appear after sexual contact with an infected partner. When in doubt, consult a healthcare provider for proper diagnosis.
Can white spots on testicles be cancerous?
Testicular cancer rarely presents as white spots on the scrotum. It more typically appears as a painless lump or swelling within the testicle itself, not on the skin of the scrotum. However, any unusual changes to the testicles should be evaluated by a doctor.
How long do white spots on testicles last?
The duration varies depending on the cause. Temporary conditions like pimples or ingrown hairs typically resolve within a week or two. Chronic conditions like Fordyce spots are permanent but harmless. Infections may persist until properly treated.
Can certain medications cause white spots on balls?
Some medications, particularly those that affect the immune system or hormone levels, might make you more susceptible to skin conditions that can present as white spots. If you notice new spots after starting a medication, consult your doctor.
Remember, while finding white spots on your testicles might be concerning, in most cases, they’re completely harmless. When in doubt, a healthcare provider can offer proper diagnosis and peace of mind.